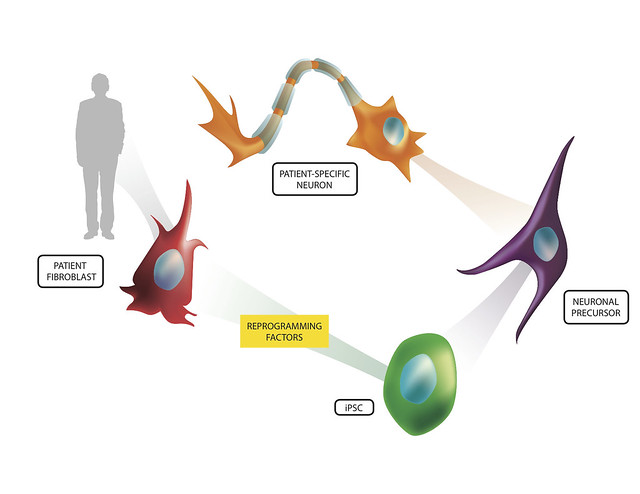
These iPSCs, once discovered, opened up those doors that ethical and moral questions shut for researchers. But, it was clear the iPSCs are different than hESCs and researchers had a fair bit of work in front of them to make sure that the iPSCs were at least comparable in the flexibility and thus utility of hESCs. This largely entailed experimenting with different environments and factors that the researchers would submit the cells to in order to create iPSCs. Eventually, researchers were able to derive iPSCs from more than just human skin cells (Yu et al, 2007), but other cells such as human urine cells (Zhou et al, 2012). As researchers have improved on these techniques, researchers like Morizane et al (2013) set out to investigate the quality of these iPSCs by injecting them into animals to investigate the utility of iPSCs as well as evaluate the benefits stem cells from one's own body may have on graft rejection or lack thereof.
In the study by Morizane et al (2013), the researchers used a primate model in order to evaluate the ability for autologous iPSCs and allogenic iPSCs to generate an immune response and engraft dopamine neurons in the primate midbrain. Like any other transplantation the immune system is an important player in the ability for the limb, cell, organ, etc. to engraft and become functional in the body. If recognized by certain immune cells in the body, the body can start attacking the transplant, reject it, and potentially damage the surrounding area in the process.
 |
| http://www.flickr.com/photos/lalande/6775578122/ |
In order to generate these iPSCs, the authors used two different techniques to induce pluripotency. One technique was to use retroviral vectors to incorporate specific genes in the cell genome via a virus that would cause it to become an iPSC. Another technique was the use of episomal vectors, where the genes are incorporated into the nucleus of the cell in circular DNA loops that also can be transcribed. Both techniques involve a growth process that is mediated (and manipulated by the researchers) by the media in which the cell cultures differentiate. In this case, the researchers wished for these cells to become dopaminergic midbrain progenitor neurons. In addition to the normal genes to create neural precursors, they added green florescent protein (GFP) to the iPSCs so that they could analyze the donor cell engraftment post-mortem in brain slices. Once they submitted the cells to the differing environments, they analyzed the cells through flow cytometry which can identify the type and state of cells by analyzing what markers are present on the cells. They confirmed that the cells were now dopaminergic progenitor neurons that were fit for transplantation. One of the most important markers was the expression of the major histocompatibility complex class I (MHC-I) on the donor cells which was found to be present in low levels on the neurons. For the autografts, the MHC-I for the donor and the recipient would be identical, but would be different for the allografts (confirmed by flow cytometry). This is important as this is the molecule through which the immune system can identify cells that are 'self' and 'foreign' and thus decide to elicit a response or not to that cell.
In order to make sure they were injecting these cells into the desired midbrain location, the putamen, the researchers used MRI (magnetic resonance imaging) to get the exact coordinates for each animal. The cells were injected in multiple sites in the right putamen (totaling 800,000 cells) and - in order to set a within-animal control - the media the cells were grown in were injected in the same number of sites in the left putamen.
In order to study of how the immune system was responding to the injected cells over time, they conducted positron emission tomography (PET) scans over the course of 3.5-4 months. These scans use radioactive isotopes to watch the travel of a specific substance in the body, and they chose a radioactive carbon isotope that has been shown to bind to proteins on microglia - the resident immune cell in the brain. Only one monkey showed an remarkable increase in the microglia marker, and that was an allografted monkey. Further, the post-mortem analysis of the brain slices showed that the adaptive immune response marker (MHC-II) was also present in the allografted animals and not the autografted animals.
Results showed that both the autograft and allograft techniques had surviving dopamine neurons, but with autologous animals having more. Further, the injected cells in the midbrain adopted the midbrain characteristics of dopamine neurons, showing that the engraftments were functional. As described above, PET scans did find that there was increased microglial activity in some allografted animals, but no such activity in the autografted animals. Further, brain slice analysis showed an increase in CD45+ cells in the allografted animals - including CD3+ and CD8+ killer T cells. These data suggest that an acquired immune response was elicited only in the allografted monkey brain.
Overall, it was evident that the autologous iPSCs were more efficiently grafted in the primates. With this in mind, the authors noted some future directions that could be investigated, such as instead of the more labor-intensive autograft procedure, perhaps allograft banks of differing MHC-I types could be made for any future iPSC transplantation. This way, the cells would be pre-prepared and have identical MHC alleles so that the immune response would be like the autologous type without the labor necessary for each new patient.
I thought this study was very well done, and provided one of the first accounts for evaluating iPSC treatment in primates. One concern I had of the study was that they did find astrocytes that were injected in the brain slices. This shows that the protocol to differentiate their iPSCs into midbrain neurons was not completely effective and could be improved upon. On the other side of the coin, did the astrocytes help the neurons engraft functionally? Astrocytes are well-known for their support structurally and biochemically for neurons, so perhaps future research may investigate advantages or disadvantages for co-injections. Another concern I had was the low concentration of MHC-I on the neurons. Although MHC-I concentrations were noted to increased with IFN-gamma (which will be in increased levels by the nature of the injection), these cells could potentially trigger Natural Killer (NK) cell activation as those cells recognize cells without MHC-I complexes and kill them. Although no NK cells were observed in the brain slices, maybe in less immunoprivileged sites, making sure MHC-I was in high concentration would prove to be beneficial in the number of engrafted cells. Lastly, it was encouraging that there was a 3.5-4 month delay before the brain slice analysis, but it leaves one to wonder - as with any type of cell injections - would a longer delay elicit tumorigenesis?
In the end, this study is very encouraging for any future of neurodegenerative disease treatment. Research like this excites both the neuroscience community and immunologists alike as autologous transplantation becomes closer and closer to reality. Perhaps not too far down the road, Parkinson's patients will be generating their own skin-derived stem cells to help replace their degenerating dopaminergic midbrain neurons.
References:
Morizane A, Doi D, Kikuchi T, Okita K, Hotta A, Kawasaki T, Hayashi T, Onoe H, Shiina T, Yamanaka S, and Takahashi J. Direct Comparison of Autologous and Allogenic Transplantation of iPSC-Derived Neural Cells in the Brain of a Nonhuman Primate. Stem Cell Reports 1:283-292 (2013).
Yu J, Vodyanik MA, SMuga-Otto K, Antosiewicz-Bourget J, Frane JL, Tian S, Nie J, Jonsdottir GA, Ruotti V, Stewar R, Slukvin LL, Thomson JA. Induced pluripotent stem cell lines derived from human somatic cells. Science 318(5858): 1917-20 (2007).
Zhou, T, Benda C, Dunzinger S, Huang Y, Cy Ho, J, Yang J, Wang Y, Zhang Y, Zhuang Q, Li Y, Bao X, Tse HF, Grillari J, Gillari-Voglauer R, Pei D, and Esteban MA. Generation of human induced pluripotent stem cells from urine samples. Nature Protocols 7: 2080-2089 (2012).
No comments:
Post a Comment