In Response to
Dahal, B., Lin, S. C., Carey, B. D., Jacobs, J. L., Dinman, J. D., van Hoek, M. L., ... & Kehn-Hall, K. (2020). EGR1 upregulation following Venezuelan equine encephalitis virus infection is regulated by ERK and PERK pathways contributing to cell death. Virology, 539, 121-128.
The Venezuelan Equine Encephalitis Virus (VEEV) is a rare, but debilitating virus that can cause severe neurological symptoms in both humans and horses. VEEV is a positive-sense single-stranded RNA Alphavirus from the Togaviridae virus family. There are fourteen different strains of VEEV of which four, IA/B, IC, ID, and IE, can infect humans (Aguliar et al. 2011). The virus is spread to humans primarily through mosquito bites or contact with infected horses (Aguliar et al. 2011). VEEV infections occur in two stages. During the first stage, the virus infects the periphery organs, in particular, glands such as the lymph nodes and the spleen. During this stage, patients typically experience symptoms such as fever, vomiting, and diarrhea. The second, and more serious, stage of the infection begins when the virus progresses to the central nervous system (CNS). Infection in the CNS causes encephalitis, inflammation of the brain. If the patient develops encephalitis, they may experience convulsions or feel disorientated. Sometimes encephalitis can lead to death which occurs in around 1% of people infected with VEEV (Zacks and Paessler, 2010). Twelve countries in the Americas have reported outbreaks of this debilitating virus with the first documented outbreak occurring in Columbia in the 1950s (Aguliar et al. 2011).
VEEV is of concern to public health officials because of its potential use as a biochemical weapon of terror. During the Cold War, both the Soviet Union and the United States weaponized the virus by developing aerosol forms to use as a biochemical agent against enemy combatants (Davis, 1999). When the virus is in aerosol form, VEEV causes a more serious infection because it can directly infect the CNS through the olfactory system (Vogel et al., 1996). The potential for this virus to be used as a weapon of terror has prompted scientists to study the viral mechanism of the VEEV to develop drugs that prevent the debilitating neuropathology from occurring once the disease progresses to the second stage of the infection.
To gain a better understanding of how to address and prevent VEEV infection, scientists have begun investigating the changes in the brain that occur once VEEV has infected neurons. Astrocytes are one type of brain cells heavily targeted in the second stage of VEEV infection (Peng et al., 2013). Astrocytes are glial cells found in the brain that have many functions ranging from promoting CNS homeostasis to reducing brain inflammation following infection (Guttenplan and Liddelow, 2018). After VEEV infection, there is an increase in astrocyte apoptosis, cell-initiated cell death (Aronson et al., 2000). Dr. Kehn-Hall’s laboratory group at George Mason University recently released a paper in Virology which seeks to uncover the mechanism of VEEV infection that results in high levels of astrocyte apoptosis. The lab group sought to build off their previous research which showed that VEEV infection caused an increase in the level of early growth response 1 (EGR1) mRNA and proteins in astrocytes in a cancer cell line (Baer et al., 2016). EGR1 is an immediate-early gene associated with cell growth, survival, and apoptosis (Pagel and Deindl, 2011). In their 2019 paper, these researchers sought to replicate their findings in primary human astrocytes, because the primary astrocyte culture would be more reflective of what occurs in a human brain during VEEV infection. Additionally, the researchers were interested in uncovering which cellular pathways are responsible for the upregulation of ERG1 expression and, consequently, greater levels of cellular apoptosis.
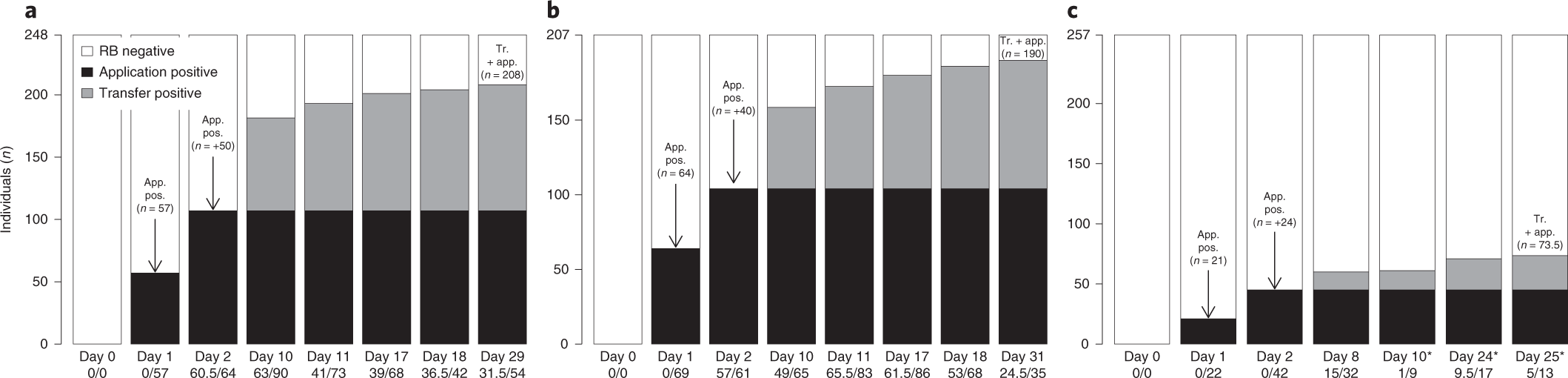
Researchers in the Kehn-Hall lab first determined whether or not ERG1 expression is elevated in primary human astrocyte cultures after VEEV infection. They tested their hypothesis by infecting primary human astrocyte cell cultures with the TC-83 strain of VEEV. TC-83 is a live attenuated strain of the VEEV virus. Live attenuated strains are forms of viruses that can infect cells, but which have been modified so they are less virulent than unmodified strains of the viruses (Lauring et al., 2010). These strains of viruses are safer for laboratory use. Following infection, the scientists ran real-time quantitative polymerase chain reactions (RT-qPCR) to measure the respective amounts of ERG1 mRNA transcript levels in the primary human astrocytes after VEEV infection. RT-qPCR measures increases in levels of mRNAs of interest compared levels of control mRNAs, which are held at reliable levels in the cell. For this experiment, ribosomal RNA was used as a control for comparing levels of ERG1 mRNA level. The Kehn-Hall laboratory found a significant upregulation of EGR1 gene expression nine hours post-infection as displayed by the increase in fold change of EGR1 mRNA transcript (Figure 1). Thus, their RT-PCR analysis of VEEV infected primary human astrocyte cultures demonstrated that VEEV infected astrocytes have increased expression of the EGR1 mRNA.

Figure 1. Quantification of EGR1 Gene Expression Following VEEV Infection in Primary Human Astrocytes. EGR1 RNA levels in primary human astrocyte cell cultures incubated with either VEEV or a control MOCK injection were quantified at 3, 6, 8, and 18 hours post-infection. Analysis was completed with RT-qPCR. Significant upregulation of ERG1 transcripts was found in VEEV infected cells 9 and 18 post-infection.
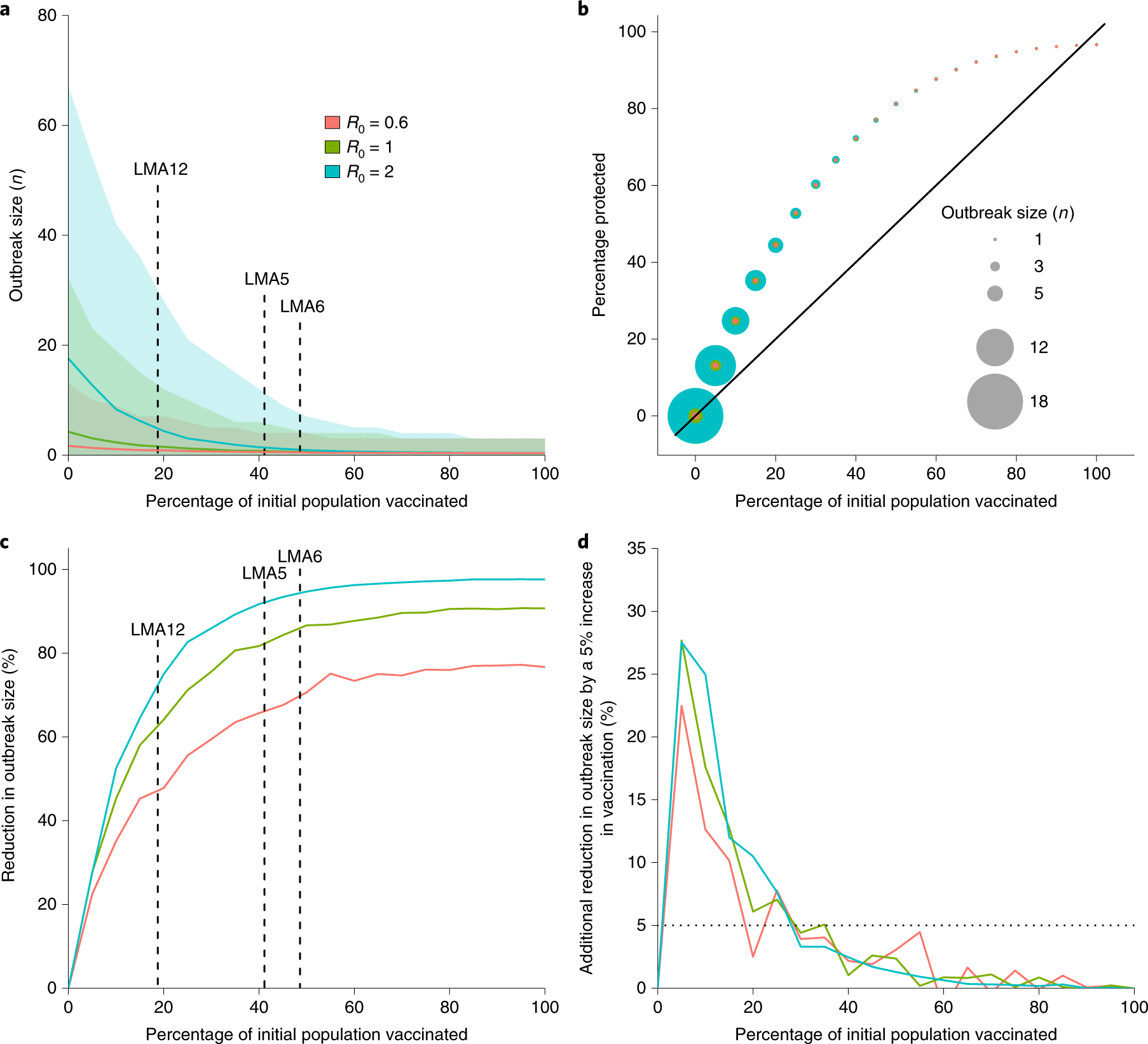
After demonstrating that EGR1 levels were elevated in astrocytes following VEEV infection, the research group wanted to assess which internal cellular pathways were responsible for the upregulation in EGR1 expression. The researchers examined four pathways previously implicated in EGR1 upregulation: the extracellular signal-regulated kinase (ERK), p38 mitogen-activated protein kinase (p38 MAPK), phosphoinositide 3-kinase (PI3K) and the protein kinase RNA-like endoplasmic reticulum kinase (PERK) pathway. The researchers infected cells with VEEV and small kinase inhibitor molecules previously shown to inhibit either the ERK, p38 MAPK, PI3K, or PERK pathway. As before, the researchers quantified the levels of EGR1 expression with RT-qPCR. Their results are displayed in figure 2. The researchers found that inhibition of the ERK and PERK pathways caused a significant decrease in EGR1 gene expression in primary astrocyte cultures infected with VEEV when compared to control cell cultures, those treated with dimethyl sulfoxide (DMSO). Inhibition of p38 MAPK did not yield any significant changes in EGR1 expression when compared to control cells. Interestingly enough, treatment with PI3K inhibitors significantly increased the expression of EGR1 gene transcripts in astrocytes treated with VEEV. The researchers posited no explanation for why PI3K inhibitors triggered a rise in EGR1 transcripts, but in the future, the researchers should investigate this finding to determine why their results were inconsistent with previous papers that found that inhibition of PI3K triggered a decrease in EGR1 gene expression (Pagel and Deindl, 2011).

Figure 2. The Impact of Pathway Inhibition on EGR1 Transcript Expression. Researchers utilized RT-qPCR to assess the difference in EGR1 transcript levels following inhibition of the ERK, p38 MAPK, PI3K, and PERK pathways. Expression of EGR1 in cells treated with inhibitors was compared to the expression of EGR1 in cells treated with DMSO, a nonreactive solution. VEEV infected cells expressions were compared to MOCK control cells expressions. Researchers found a significant decrease in ERG1 expression following inhibition of the ERK and PERK pathways.
After identifying which cellular pathways were responsible for the upregulation of EGR1 after VEEV infection, the researchers examined whether inhibition of the PERK or ERK pathway would reduce astrocyte apoptosis and, consequently, increase cell viability. To test this hypothesis, the researchers used small interference RNAs (siRNAs) to target the ERK and PERK pathways in primary astrocytes before infecting the cells with VEEV. siRNAs target mature RNA sequences in cells by binding to commentary RNA base-pair sequences found in the targeted RNA sequence. siRNAs are designed in laboratories to fuse with specific mRNA and thus can reliably and consistently inhibit the expression of target molecules. Following binding, the siRNA directs the cleavage of the targeted RNA, effectively removing the RNA sequence from the cell (Lopez-Sierra and Esteller, 2012). Researchers transfected cells with siRNAs that targeted the ERK pathway, the PERK pathway and a negative siRNA which was used as a control. Cell viability assays measured ATP production in cells as a proxy measurement for cell viability; increased ATP production was used to demonstrated increased cell viability. The researchers also performed caspase 3/7 assays to assess the levels of apoptosis occurring in the primary human astrocyte cultures. Caspase 3/7 is a molecule released in late-stage apoptosis; an upregulation of this molecule in cell cultures indicates that a greater level of apoptosis is occurring in the cell. (Carrasco et al., 2003). Through these two assays, the researchers found that inhibition of both the ERK and PERK pathways increased astrocyte cell viability and decreased caspase 3/7 activity following VEEV infection (Figure 3). These results suggest that these two cellular pathways are significantly involved in triggering astrocyte apoptosis following VEEV infection.

Figure 3. Cell Viability and Caspase 3/7 Assays in VEEV infected Cells following ERK and PERK Inhibition. Levels of astrocyte viability and apoptosis following VEEV infection were analyzed through cell viability and caspase 3/7 assays. In cell cultures where ERK and PERK pathways were inhibited, there was a significant increase in cell viability and a decrease in caspase 3/7 activity. These results suggest that ERK and PERK pathways induce apoptosis in human astrocytes following VEEV infection.
Based on their experimental data, the researchers in the Kehn-Hall laboratory developed a model for the upregulation in EGR1 expression and resulting in apoptosis increase in astrocytes following VEEV infection (Figure 4). The researchers proposed that when VEEV infects the cell, the ERK pathway is directly triggered and begins to stimulate the expression of ERG1. While ERK is directly upregulated by VEEV, the virus’s proteins accumulate in the host cell’s endoplasmic reticulum which the cell recognizes as foreign proteins. The presence of foreign proteins causes the cell to activate the unfolded protein response (UPR) which stimulates the PERK pathway. The PERK pathway interacts with the ERK pathway and also increases the amount of EGR1 expression. Increased EGR1 expression ultimately leads to an increase in apoptosis in astrocytes.

Figure 4. Proposed Model for Human Astrocyte Apoptosis Upregulation Following VEEV Infection. Researchers at the Kehn-Hall lab proposed that VEEV infection directly triggers the ERK pathway and indirectly triggers the PERK pathway through activation of the cell’s unfolded protein response (UPR). Both of these pathways stimulate greater expression of the EGR1 gene which triggers apoptosis in human astrocytes.
Looking towards the future, the Kehn-Hall lab is interested in understanding why ERG1 expression causes an increase in cellular apoptosis. There are no experimentally verified mechanisms that explain why an upregulation of EGR1 causes an increase in apoptosis. The experimenters have theorized that ERG1 stimulates other genes in the cell which directly cause apoptosis, but they need to perform more research to support their theory on ERG1’s role in apoptosis. Beyond uncovering the role of ERG1 in apoptosis, the researchers need to develop an improved way to test the influence of ERK on ERG1 transcript expression and caspase 3/7 activity. In their RT-qPCR analysis of ERG1 transcripts and caspase 3/7 assays following ERK inhibition, the reduction in ERG1 expression and caspase 3/7 activity in the VEEV infected cells was remarkably similar to the reduction in ERG1 expression and caspase activity in the control cells. Thus, it is imperative for the researchers to perform additional tests on the influence of ERK inhibition on ERG1 expression to verify that the pathway does stimulate the gene expression following VEEV infection and not just generally cause a greater expression of all genes in astrocytes. On a broader level, the VEEV community should investigate how the rates of the disease could potentially increase with the dawn of climate change. VEEV is spread through mosquito vectors, and currently, climate change has caused a shift global temperature that facilitates the breeding of mosquitos (Aguliar et al. 2011). A global rise in the mosquito population could potentially trigger a massive surge in mosquito-transmitted illnesses such as VEEV. Scientists must continue to perform research on diseases like VEEV to prepare the global community for an exponential increase in mosquito-spread diseases.
References
Aguilar, P. V., Estrada-Franco, J. G., Navarro-Lopez, R., Ferro, C., Haddow, A. D., & Weaver, S. C. (2011). Endemic Venezuelan equine encephalitis in the Americas: hidden under the dengue umbrella. Future virology, 6(6), 721-740.
Aronson, J. F., Grieder, F. B., Davis, N. L., Charles, P. C., Knott, T., Brown, K., & Johnston, R. E. (2000). A single-site mutant and revertants arising in vivo define early steps in the pathogenesis of Venezuelan equine encephalitis virus. Virology, 270(1), 111-123.
Baer, A., Lundberg, L., Swales, D., Waybright, N., Pinkham, C., Dinman, J. D., ... & Kehn-Hall, K. (2016). Venezuelan equine encephalitis virus induces apoptosis through the unfolded protein response activation of EGR1. Journal of virology, 90(7), 3558-3572.
Carrasco, R. A., Stamm, N. B., & Patel, B. K. (2003). One-step cellular caspase-3/7 assay. Biotechniques, 34(5), 1064-1067.
Davis, C. J. (1999). Nuclear blindness: An overview of the biological weapons programs of the former Soviet Union and Iraq. Emerging infectious diseases, 5(4), 509.
Guttenplan, K. A., & Liddelow, S. A. (2018). Astrocytes and microglia: Models and tools. Journal of Experimental Medicine, 216(1), 71-83.
Lauring, A. S., Jones, J. O., & Andino, R. (2010). Rationalizing the development of live attenuated virus vaccines. Nature biotechnology, 28(6), 573.
Lopez-Serra, P., & Esteller, M. (2012). DNA methylation-associated silencing of tumor-suppressor microRNAs in cancer. Oncogene, 31(13), 1609.
Pagel, J. I., & Deindl, E. (2011). Early growth response 1—a transcription factor in the crossfire of signal transduction cascades.
Peng, B. H., Borisevich, V., Popov, V. L., Zacks, M. A., Estes, D. M., Campbell, G. A., & Paessler, S. (2013). Production of IL-8, IL-17, IFN-gamma and IP-10 in human astrocytes correlates with alphavirus attenuation. Veterinary microbiology, 163(3-4), 223-234.
Vogel, P., Abplanalp, D., Kell, W., Ibrahim, M. S., Downs, M. B., Pratt, W. D., & Davis, K. J. (1996). Venezuelan equine encephalitis in BALB/c mice: kinetic analysis of central nervous system infection following aerosol or subcutaneous inoculation. Archives of pathology & laboratory medicine, 120(2), 164-172.
Zacks, M. A., & Paessler, S. (2010). Encephalitic alphaviruses. Veterinary microbiology, 140(3-4), 281-286.