Among the many types of autoimmune disorders perhaps the most interesting and least understood disorders are those in which the immune system attacks the central nervous system. Multiple Sclerosis (MS) is an autoimmune disorder in which invading lymphocytes attack the protective insulation of neurons called myelin. The disease is neurodegenerative and leaves patients wheelchair bound within a few short decades of its clinical presentation. While scientists have unraveled many of the pathological hallmarks of the disease, its cause and effective treatment remain elusive.
 |
| Lesions in an MS brain |
A new study in the Journal of Immunology published this
month investigates the types of white blood cells that are involved in the
attack of white matter (myelin) in the brain.
Previous studies have identified a subset of Helper T cells as a major
cause of the pro-inflammatory environment which leads to the ultimate
degeneration which is characteristic of the disease. These cells are part of the adaptive immune
systems which targets very specific pathogens and in some cases (like in MS) accidentally
targets cells or proteins that are part of the body’s normal function. However, the new article presents data that
demonstrates that innate immune cells called neutrophils may be playing a role
in the initial stages of the disease. These innate immune cells are non-specific to
any particular protein but instead identify and attack cells with general
molecular patterns associated with invading pathogens. This is the first time it has been shown that
neutrophils have been involved in MS.
In order to show the involvement of neutrophils,
neuroimmunologists used an animal model of Multiple Sclerosis called
Experimental Autoimmune Encephalomyelitis (EAE) in which mice are immunized
with a myelin protein so that the immune system will begin to attack the myelin
found in the brain. After immunizing the
mice, the scientists used an antibody-mediated depletion of neutrophils prior
to the clinical onset of the disease.
And what did they find? Turns out
when neutrophils are depleted the disease onset is delayed and continual
depletion of neutrophils will stop the disease course so long as depletion
continues. This result is striking but
also brought up more questions than it answered. How are neutrophils contributing to the
disease? Why was this not found earlier?
How do we know that they only depleted neutrophils and did not wipe out
large portions of the immune system instead? These questions prompted
scientists to probe deeper.
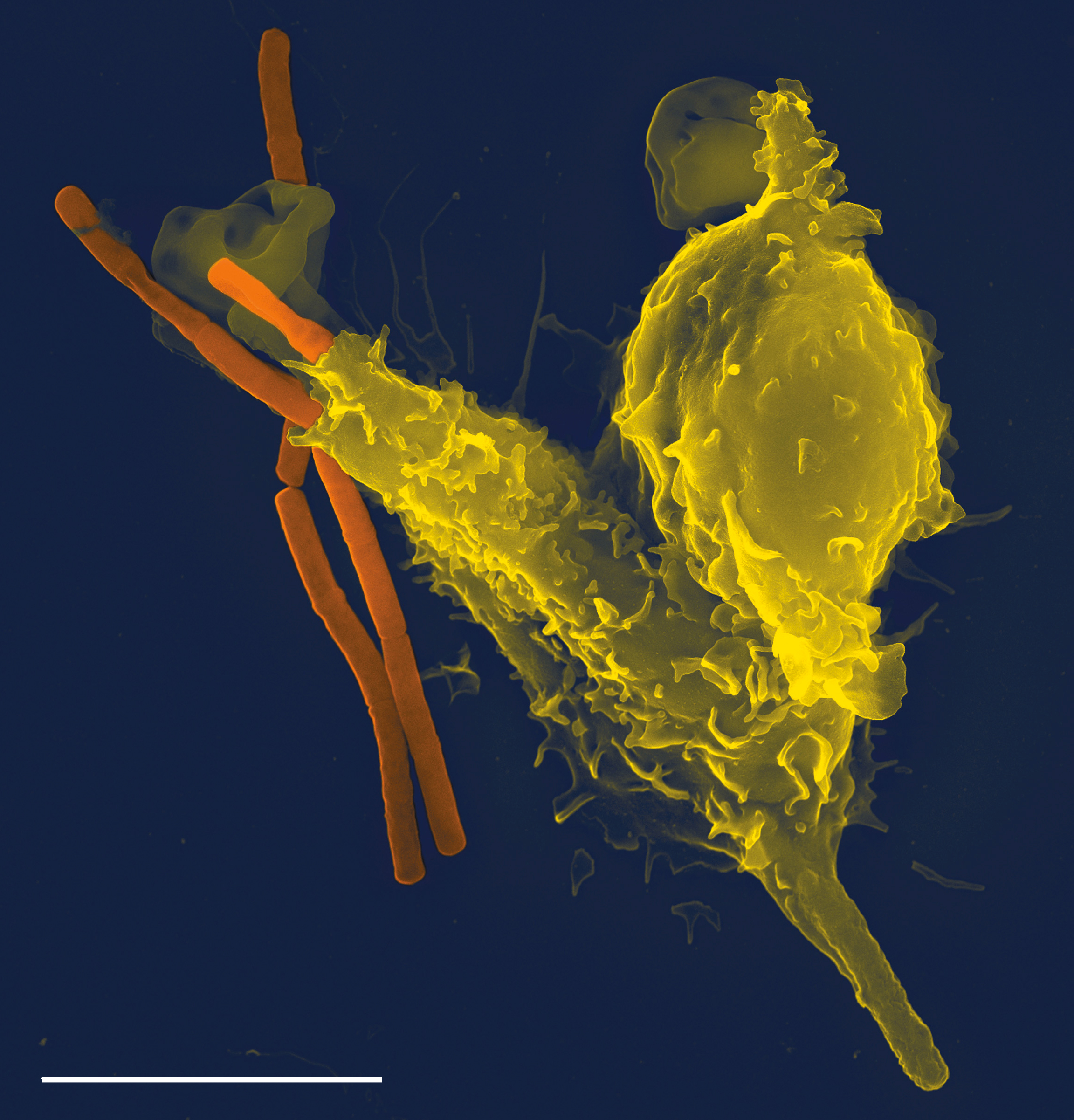 |
| Above a Neutrophil is shown in yellow |
Following antibody treatment of neutrophils the remaining
lymphocytes were classified and measured via flow cytometry. Despite the
attenuation of clinical EAE symptoms differentiation of Th1 and Th17 cells were
unchanged. Since the depletion of these
innate immune cells did not affect the amount or function of the T cells implicated
in MS then they must be providing some other means of disease
contribution. Using inhbitors and
genetic knockouts EAE immunized mice were deprived of neutrophil related
enzymes such as MPO which increases endothelial permeability and ELANE which
creates a pro-inflammatory environment and it was found that neither of these
modifications changed disease progression in the way total neutrophil depletion
had. So the question remain, what aspect
of neutrophils was contributing to demyelination? It was found that neutrophils isolated from
the CNS were a primary source of cytokines (immune signaling molecules) which
may be contributing to the development of other more dangerous immune
responses. Specifically the cytokines
TNF-alpha, Interferon-gamma, Interleukin-6, and Interleukin-12 were produced by
neutrophils which could lead to the maturation of specialized Antigen
Presenting Cells in the brain which provide crucial information to the Th cells
about pathogens. Indeed, when the APC’s
from inside the brain of mice were isolated and analyzed it was found that
neutrophils from the brain caused an increased expression of antigens on APCs
yet neutrophils from bone marrow did not have the same affect. The major consequence of this finding is that
some component of neutrophils is increasing the maturation of these cells which
ultimately stimulate T cells to destroy myelin.
Perhaps even more interesting is
that the blockade of these cytokines still did not attenuate the course of EAE
to the same extent that complete neutrophil depletion had. The authors of the paper stress the need for
further experimentation to determine the components that illicit the change in
disease progression.
I think the real question of this article is, “Is this
relevant and applicable and if it is then how?”
The best answer I can give is well…….kinda. Don’t get me wrong I think it’s really
interesting that these innate immune cells are actually playing a role but the
paper could not find a reasonable explanation for the changes they found. However, even more than the fact that they
had no definitive answer is the fact that even iof they did how would this help
MS patients? The authors only delayed
the onset of the disease for a short amount of time and any extension of that
delay means knocking out neutrophils indefinitely. This is not a reasonable thing to do in
humans considering neutrophils comprise so much of the immune system. Additionally, the current MS treatments have
shown that even delaying disease onset and progression is (and I’m sorry)
futile. The best current MS treatments work to diminish the immune system and while there may be improvement in the
first few years following clinical diagnosis, in the long term (a few decades)
there is no difference between treated and untreated patients. What the field needs is to look for permanent
solutions either through more effective treatments or by examining the
autoimmune origin of the disease and work to reverse the process. While
I commend this article for finding that neutrophils might be a contributing
factor it doesn’t contribute much to the field beyond the scope of “More
research needs to be done”. I can only
hope that I’m completely wrong and this finding propels the field forward but
for now I’m unconvinced.
Primary Source:
Secondary Sources:
No comments:
Post a Comment