In
my experience, the close of the semester and the
beginning of the holiday season generally coincides with a rapid collapse into
illness brought on by lack of sleep, constant stress, poor nutrition and far
too much time spent in the library away from natural light. Unfortunately, many times this mental
and physical collapse corresponds with an actual illness: the flu. Even though I was one of the first on
campus to get a flu shot (did you get yours?), I could still possibly contract
the flu in addition to the aforementioned collapse, as each year the vaccine
producers guess which strain of flu will be most likely to spread. If they miscalculated and selected the
wrong strain, then my exhausted classmates and I
could be in for a fun-filled break.
could be in for a fun-filled break.
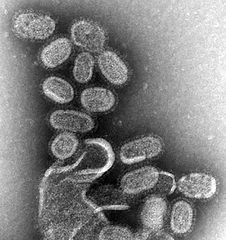
A
recent study
uniting scientists from the
University of Maryland School of Medicine, Columbia University, the University of Connecticut Health Center and the University of Pennsylvania School of Medicine identified a new class of memory CD4 T cells, in the lungs; research based on this discovery could eventually lead to a flu vaccine that would remove the possibility of my classmates and I needing to cope with the flu on top of exhaustion and stress induced illnesses. Memory cells are produced following initial exposure to a pathogen and “remember” specific components of the pathogen, in case a person is infected with the same, or highly similar, pathogen in the future. CD4 T cells, also called “helper” T cells, coordinate the adaptive immune response, by assisting B cells to produce antibodies and CD8 T cells to kill infected cells. This study utilized the identification of influenza-specific, stationary, memory CD4 T cells in the lung to examine their memory in comparison with CD4 T cells found in the spleen. This experiment was carried out with mice that were infected with a specific strain of influenza; the mice who had memory CD4 cells in their lungs only did not die, whereas the mice with CD4 T cells in their spleens seemed to have a greater likelihood of dying from the influenza, even though their T cells were found in a more diverse area and had the ability to migrate to peripheral tissue sites to encounter the infection.
University of Maryland School of Medicine, Columbia University, the University of Connecticut Health Center and the University of Pennsylvania School of Medicine identified a new class of memory CD4 T cells, in the lungs; research based on this discovery could eventually lead to a flu vaccine that would remove the possibility of my classmates and I needing to cope with the flu on top of exhaustion and stress induced illnesses. Memory cells are produced following initial exposure to a pathogen and “remember” specific components of the pathogen, in case a person is infected with the same, or highly similar, pathogen in the future. CD4 T cells, also called “helper” T cells, coordinate the adaptive immune response, by assisting B cells to produce antibodies and CD8 T cells to kill infected cells. This study utilized the identification of influenza-specific, stationary, memory CD4 T cells in the lung to examine their memory in comparison with CD4 T cells found in the spleen. This experiment was carried out with mice that were infected with a specific strain of influenza; the mice who had memory CD4 cells in their lungs only did not die, whereas the mice with CD4 T cells in their spleens seemed to have a greater likelihood of dying from the influenza, even though their T cells were found in a more diverse area and had the ability to migrate to peripheral tissue sites to encounter the infection.
Generally, if T cells have the
chance to migrate to the peripheral tissues to directly engage the infection,
then they will be more effective at attacking and removing the pathogen. The memory T cells produced can then
remain in the tissues which had been infected or they can move to other areas
of the body until they are called into action upon the return of the
pathogen. In order to design a
vaccine that can effectively target the most common tissue infection site for a
specific pathogen, it must be known which location for the memory T cells is
most effective.
The hypothesis tested in this study
was that the specific tissue site of the CD4 T cells would play a key role in
determining their homing abilities and thus their success at protecting the
infected mouse from dying from the influenza strain used in the experiment,
H1N1. The lung memory CD4 T cells
were found to produce a greater amount of IFN-gamma, an important inflammatory
messanger, than the spleen memory CD4 T cells, while the spleen memory CD4 T
cells had a greater amount of IL-2 producers than the lung memory CD4
cells. These values show that
resident memory populations may function independently from the specifics of
the antigen. The lung memory CD4 T
cells remained in the lung and contain so called “zip codes” which let them
identify the tissue they are supposed to be in and concentrate their efforts
specifically in the site of the infection; the spleen memory CD4 T cells do not
have these zip codes. An additional
comparison between lung memory CD4 T cells and lung memory CD8 T cells revealed
the special zip code feature of the CD4 T cells, as the CD8 cells may migrate
to lymph tissues and non-lymph tissues.
Because of the homing device, the lung memory CD4 T cells have increased
protective abilities; all the mice containing just this type of T cell
survived, whereas the spleen mice, whose CD4 T cells could migrate to other
tissues, were not as fortunate.
This newly discovered CD4 T cell
offers wonderful protection against respiratory infections, including
influenza. Their protective
capabilities are due to their “zip
code” homing behavior, placing them
directly in the site of the infection.
Further study proposed by these researchers would be to examine how knowledge
of compartmentalized CD4 T cells can be applied to vaccines. If a vaccine can be made to
target a specific tissue and generate specific memory T cell that will remain
in that tissue, then it will be far easier to combat specific strains of antigens. This would be especially useful for
influenza. Hopefully this will
become a reality and the flu shot will be guaranteed to prevent the flu (though
students may still have to deal with the end of semester collapse).
Teijaro, J. R., Turner, D., Pham, Q., Wherry, E. J.,
Lefrancois, L., & Farber, D. L. (2011). Cutting edge:
tissue-retentive lung memory CD3 T cells mediate optimal protection to
respiratory virus infection. The Journal of Immunology, 187, 5510-5514.
Post by Jessie Solcz
Hey guys,
ReplyDeleteYou have provided a very good site to knowing about Memory CD4 T cells. These T cells allow to identify specific foreign entities and eliminate them from the body, which is presented with a piece of the pathogen known as an antigen which can bind to the TCR...
Apoptosis Detection